Ghana's Psychiatric Shortage: Implications For Mental Healthcare Access

Table of Contents
The Extent of the Psychiatric Shortage in Ghana
H3: Insufficient Number of Psychiatrists
Ghana's mental healthcare system is severely strained by a critical lack of psychiatrists. Precise figures are challenging to obtain, but estimates suggest a drastically insufficient number of psychiatrists per capita compared to international standards. The World Health Organization (WHO) recommends a minimum ratio of psychiatrists to population, a benchmark Ghana falls far short of.
- Specific Numbers: While precise data is limited, reports indicate Ghana has significantly fewer than 1 psychiatrist per 100,000 people, compared to the WHO's recommended ratio, which varies depending on the context but generally necessitates a far higher number. This drastic disparity highlights the immense scale of the problem.
- Comparison to WHO Recommendations: Ghana's psychiatrist-to-population ratio is among the lowest globally, underscoring the urgent need for increased investment in mental health infrastructure and workforce development. The disparity results in severe limitations on the availability of specialist psychiatric care.
- Regional Disparities: The shortage is not evenly distributed. Urban areas may have slightly better access, though still inadequate, while rural communities face even greater challenges accessing specialist psychiatric care, exacerbating existing health inequalities. This uneven distribution worsens the situation for vulnerable populations.
H3: Lack of Other Mental Healthcare Professionals
The shortage extends beyond psychiatrists, impacting the entire mental healthcare workforce. There's a significant deficit of psychologists, psychiatric nurses, and other essential mental health workers. This lack of skilled professionals contributes to the inability to provide comprehensive mental healthcare.
- Specific Numbers (where available): Data on the numbers of psychologists and psychiatric nurses is scarce, but anecdotal evidence from healthcare professionals and NGOs strongly suggests a significant shortage of these professionals as well, creating bottlenecks across the entire system.
- Consequences of the Shortage: The lack of support staff means existing psychiatrists are overburdened, leading to longer waiting times, reduced quality of care, and limited capacity for effective treatment. It also hampers the development of integrated mental health services.
- Geographical Distribution Issues: The scarcity of psychologists and nurses mirrors the psychiatrist shortage in its uneven geographical distribution. Rural communities are disproportionately affected, facing a severe lack of readily available support, increasing the vulnerability of people living in these areas.
Impact on Access to Mental Healthcare Services
H3: Increased Waiting Times and Treatment Delays
The consequence of the limited number of mental health professionals is dramatically increased waiting times. Individuals seeking mental healthcare often face delays of several months, sometimes even years, before accessing treatment.
- Examples of Delays: Many individuals report waiting months for initial assessments, hindering early intervention and increasing the severity of symptoms. Access to ongoing therapy or medication management is further delayed.
- Impact on Treatment Outcomes: Delayed access leads to poorer treatment outcomes, increased hospitalizations, and higher rates of disability. Early intervention is crucial for effective management of many mental illnesses, and its delay has severe consequences.
- Consequences for Individuals with Severe Mental Illness: Individuals with severe mental illnesses are particularly vulnerable to the consequences of delayed treatment. Delays can lead to relapses, crises, and increased societal costs.
H3: Geographic Barriers to Access
Geographical location significantly impacts access to mental healthcare services. Individuals in rural areas, who already face challenges in accessing basic healthcare, struggle even more to receive mental health support.
- Limited Availability of Services: Rural areas often lack trained mental health professionals and necessary facilities. The existing services are frequently overwhelmed and unable to meet the demand.
- Transportation Challenges: Limited transportation options, poor road infrastructure, and financial constraints create significant barriers for individuals needing to travel long distances for specialized care.
- Lack of Awareness and Stigma: Stigma surrounding mental illness is prevalent in many rural communities, hindering help-seeking behaviors and creating additional barriers to access. A lack of awareness about available services also contributes to the issue.
H3: Financial Barriers to Access
The high cost of mental healthcare is a major obstacle to access. Consultations, medication, and therapy sessions can be prohibitively expensive for many Ghanaians, particularly those from low socioeconomic backgrounds.
- Cost of Consultations: The cost of consultations with psychiatrists and other mental health professionals can be substantial, representing a significant portion of an individual’s income.
- Medication Costs: The ongoing cost of medication is a considerable burden for many individuals and families, leading to non-adherence with prescribed treatments.
- Affordability for Different Socioeconomic Groups: The financial barriers disproportionately affect vulnerable populations, perpetuating health inequalities and preventing many from accessing the mental healthcare they need.
- Impact on Treatment Adherence: The high cost of treatment can lead to individuals interrupting or discontinuing treatment, undermining treatment effectiveness.
Potential Solutions and Strategies
H3: Investment in Training and Education
Addressing Ghana's psychiatric shortage requires significant investment in training and education to expand the mental health workforce.
- Expanding Training Programs: Ghana needs to expand its existing training programs for psychiatrists, psychologists, and other mental health professionals to increase the number of qualified practitioners.
- Scholarships and Financial Aid: Offering scholarships and financial aid can incentivize talented individuals to pursue careers in mental healthcare, overcoming financial barriers to entry.
- Collaboration with International Organizations: Collaborating with international organizations can provide valuable expertise, resources, and funding to support training programs.
H3: Integration of Mental Healthcare into Primary Care
Integrating mental healthcare into primary care settings can significantly improve accessibility, especially in rural areas.
- Training Primary Care Physicians: Equipping primary care physicians with basic mental health training allows them to screen for mental health issues, provide initial support, and refer patients to specialists when necessary.
- Establishing Referral Systems: Clear and efficient referral systems are essential to ensure individuals can access specialist care promptly.
- Increasing Awareness Among Primary Care Providers: Raising awareness among primary care providers about mental health issues and available resources is crucial for successful integration.
H3: Addressing Stigma and Promoting Mental Health Awareness
Reducing the stigma associated with mental illness and increasing awareness is vital in encouraging help-seeking behavior.
- Public Awareness Campaigns: Launching public awareness campaigns can help destigmatize mental illness, educating the population about common mental health conditions and available support services.
- Educational Initiatives: Including mental health education in schools and community settings can foster a culture of understanding and support.
- Community Engagement Programs: Involving communities in mental health initiatives fosters a sense of ownership and responsibility, encouraging help-seeking and reducing stigma.
H3: Policy and Regulatory Reforms
Supportive government policies and regulatory frameworks are crucial for sustainable improvements in mental healthcare access.
- Increased Government Funding: Increased government funding is essential for establishing and maintaining mental health services, including training programs, infrastructure, and medication supplies.
- Development of National Mental Health Policies: Ghana needs a comprehensive national mental health policy that outlines strategies for improving access to care, addressing stigma, and promoting mental health well-being.
- Implementation of Mental Health Legislation: Enacting and implementing effective mental health legislation is necessary to protect the rights of individuals with mental illnesses and ensure the quality of care.
Conclusion
Ghana's psychiatric shortage poses a significant crisis in mental healthcare access. The insufficient number of psychiatrists and other mental health professionals leads to increased waiting times, delayed treatment, geographic barriers, and financial challenges, disproportionately affecting vulnerable populations. Addressing Ghana's psychiatric shortage requires a multi-faceted approach involving investment in training and education, integration of mental healthcare into primary care, addressing stigma, and implementing supportive policies. Addressing Ghana's psychiatric shortage is critical to ensuring the mental well-being of the nation. We must collectively work towards solutions that improve access to quality mental healthcare for all Ghanaians. Support initiatives aimed at improving mental health services in Ghana – advocate for policy changes, support training programs, and donate to relevant organizations. Let’s work together to overcome this critical challenge and ensure equitable access to mental healthcare for all.

Featured Posts
-
 Christina Aguileras New Photoshoot Fans Accuse Her Of Excessive Photoshopping
May 02, 2025
Christina Aguileras New Photoshoot Fans Accuse Her Of Excessive Photoshopping
May 02, 2025 -
 Improving Mental Health Literacy Through Education
May 02, 2025
Improving Mental Health Literacy Through Education
May 02, 2025 -
 Government Funded Mental Health Courses A Comprehensive Guide To Ignou Tiss Nimhans Programs
May 02, 2025
Government Funded Mental Health Courses A Comprehensive Guide To Ignou Tiss Nimhans Programs
May 02, 2025 -
 Dont Miss Out Underrated Ps Plus Game For January 2024
May 02, 2025
Dont Miss Out Underrated Ps Plus Game For January 2024
May 02, 2025 -
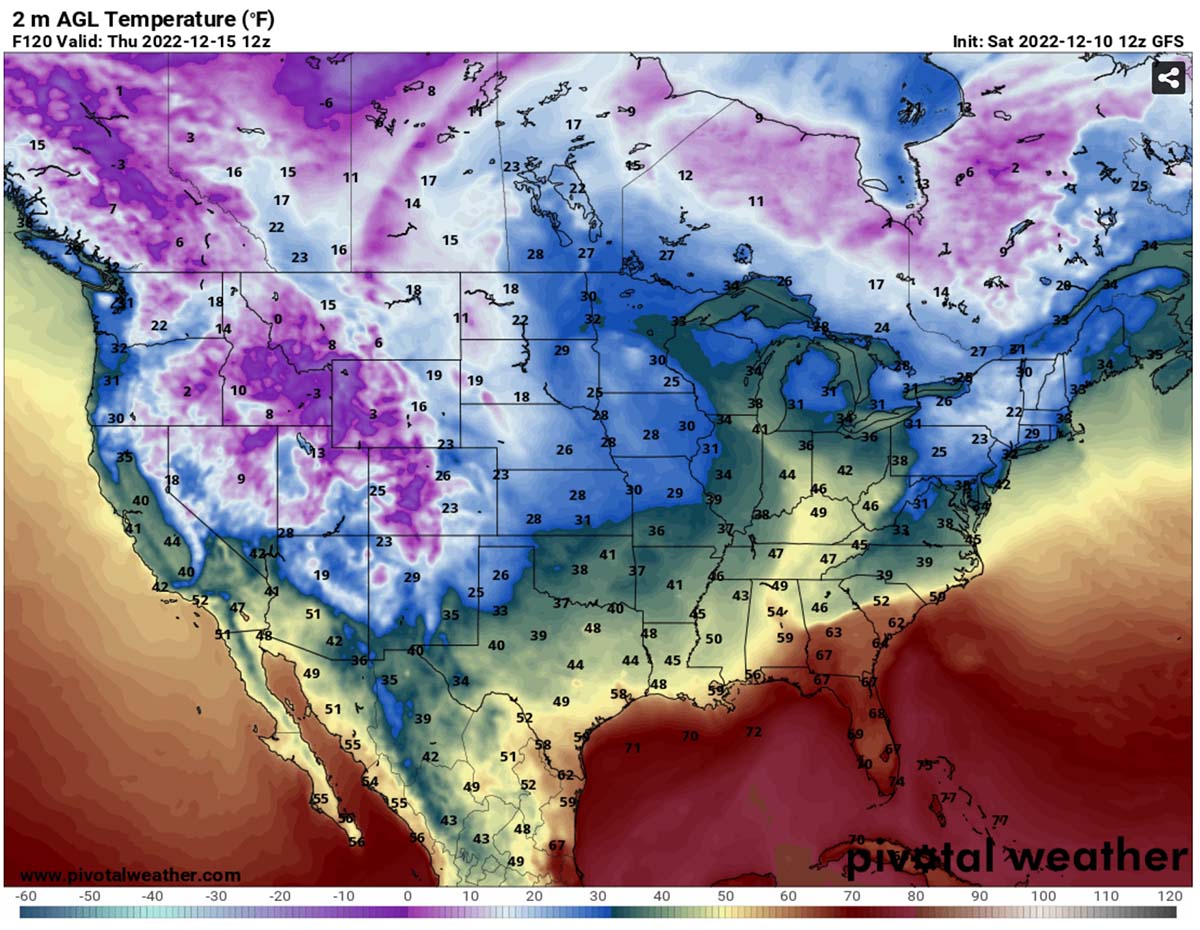 Tulsa Facing Near Blizzard Conditions Nws Forecast
May 02, 2025
Tulsa Facing Near Blizzard Conditions Nws Forecast
May 02, 2025
