The Potential Impact Of A New COVID-19 Variant On Case Rates
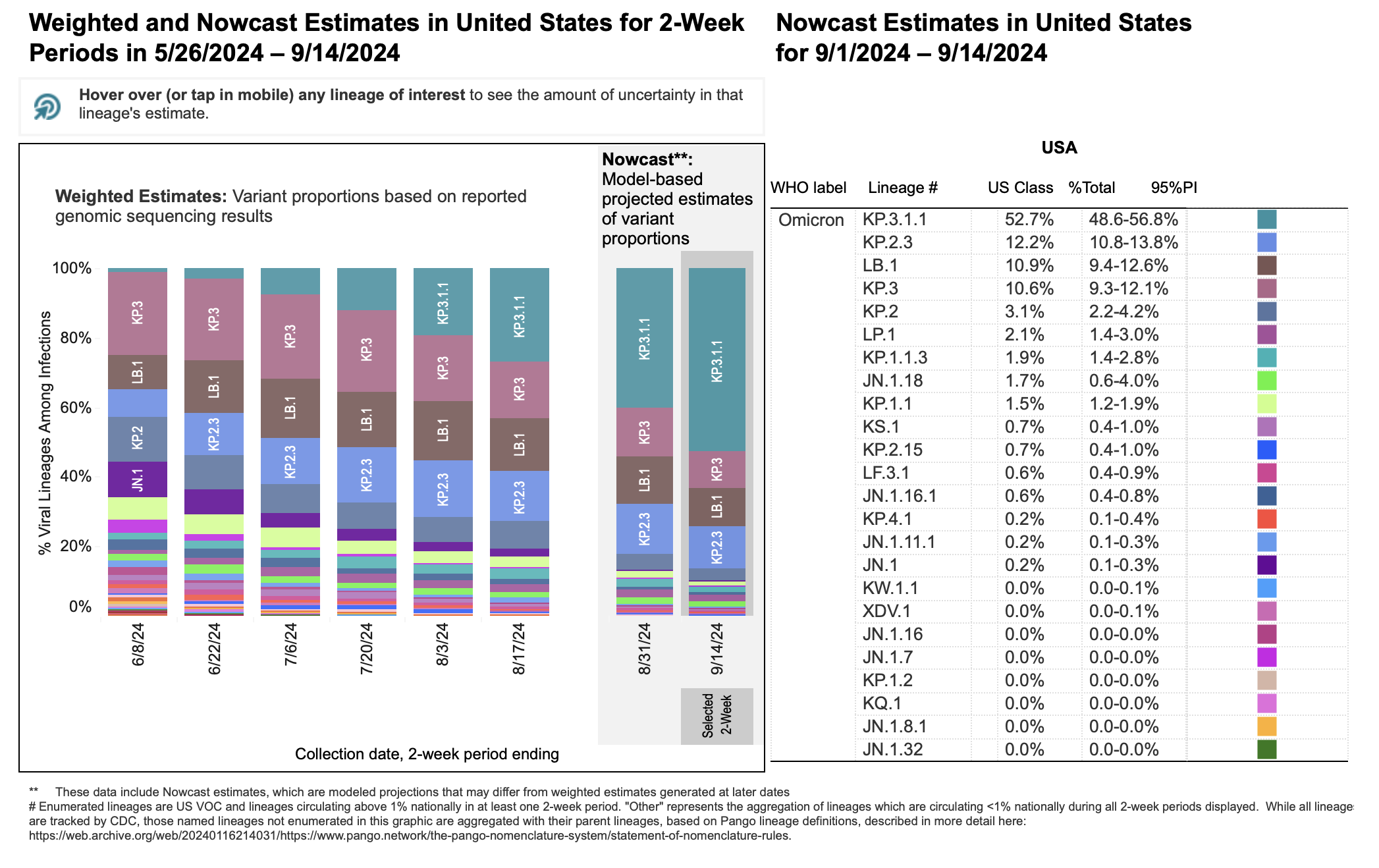
Table of Contents
Factors Influencing the Impact of a New COVID-19 Variant
The impact of a new COVID-19 variant on case rates is determined by several interconnected factors. Understanding these factors is vital for effective public health response.
Transmissibility: The Speed of Spread
Increased transmissibility, often measured by the basic reproduction number (R0), is a key determinant of how quickly a variant spreads within a population. A higher R0 value directly translates to a faster rise in case rates, potentially overwhelming healthcare systems.
- Highly Transmissible Variants: Variants like Delta and Omicron demonstrated exceptionally high transmissibility, leading to rapid surges in case rates globally. These variants spread easily due to mutations that enhance their ability to infect cells.
- Factors Contributing to Transmissibility: Mutations affecting the virus's spike protein, which allows it to bind to human cells, can significantly increase transmissibility. Increased aerosol spread, meaning the virus remains airborne for longer periods, also contributes to higher transmission rates.
- Impact on Healthcare Systems: Rapid increases in case rates due to highly transmissible variants can quickly overwhelm healthcare systems, leading to shortages of beds, staff, and resources, ultimately increasing mortality.
Severity and Mortality: The Weight of Illness
The severity of illness caused by a new variant significantly impacts hospitalizations, deaths, and overall public health burden. While case rates reflect the total number of infections, severity influences the number of severe cases requiring hospitalization and ultimately, the mortality rate.
- Comparison of Severity Across Variants: Variants have shown varying degrees of severity. Some, like Delta, were associated with more severe illness and higher hospitalization rates compared to others.
- Factors Influencing Severity: Individual factors like age, pre-existing conditions, and immune response play a significant role in determining the severity of COVID-19. The variant's intrinsic characteristics also contribute to severity.
- Hospitalization and Mortality Rates: Data on hospitalization and mortality rates associated with different variants are essential for assessing the public health impact and guiding resource allocation. Less severe variants may lead to underreporting of cases as milder infections may go undiagnosed or unreported.
Immune Evasion: The Challenge to Immunity
A variant's ability to evade the immune response, both from prior infection and vaccination, directly influences its impact on case rates. Variants that can successfully evade immunity can re-infect individuals who were previously infected or vaccinated, leading to increased transmission.
- Antibody Escape and T-Cell Responses: Some variants can escape neutralization by antibodies generated through prior infection or vaccination. However, T-cell responses, which play a role in eliminating infected cells, may offer some protection even against immune-evasive variants.
- Impact on Vaccine Effectiveness: While vaccines remain highly effective at preventing severe illness and death, their effectiveness against preventing infection can vary depending on the variant. Vaccine effectiveness can wane over time, and new variants might require updated vaccine formulations.
- Booster Shots and Updated Vaccines: Booster shots and updated vaccines are crucial for maintaining a high level of protection against new variants and reducing the risk of severe illness and hospitalization.
Predicting the Impact on Case Rates: Modeling and Surveillance
Predicting the impact of a new variant requires sophisticated tools and a robust surveillance system.
Epidemiological Modeling: Forecasting the Future
Mathematical models play a critical role in forecasting the potential spread of new variants. These models use various data inputs and algorithms to simulate the spread of the virus under different scenarios.
- Modeling Techniques: Various modeling techniques exist, including compartmental models (SIR, SEIR) and agent-based models. These models consider factors like R0, population density, contact rates, and intervention strategies.
- Limitations of Predictive Models: It's crucial to understand that these models are not perfect predictors. The accuracy of predictions depends on the quality of input data and the assumptions made in the model. Unexpected changes in behavior or unforeseen mutations can impact the model's accuracy.
- Importance of Input Data Quality: The accuracy of predictive models relies heavily on accurate and timely data, including testing rates, genomic sequencing data, hospitalization rates, and mortality data.
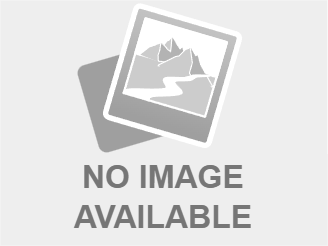
Genomic Surveillance and Variant Tracking: Monitoring the Enemy
Genomic surveillance, the process of monitoring the genetic makeup of circulating viruses, is vital for early detection and characterization of new variants. This enables a rapid response to emerging threats.
- Tracking Variant Spread: Genomic sequencing allows scientists to identify new variants, track their spread, and understand their mutations. This helps in determining their potential impact on transmission, severity, and vaccine effectiveness.
- International Collaboration: Effective variant tracking requires international collaboration in data sharing and research. Rapid sharing of genomic data allows for a quicker global response to new variants.
- Importance of Prompt Data Sharing: Timely data sharing is crucial for effective public health action. Delays in identifying and characterizing new variants can lead to increased spread and more severe consequences.
Mitigating the Impact: Public Health Strategies
Several public health strategies can effectively mitigate the impact of new COVID-19 variants on case rates.
Vaccination and Boosters: The Primary Defense
Vaccination remains a cornerstone of COVID-19 prevention and control. While vaccines may not always prevent infection, they significantly reduce the risk of severe illness, hospitalization, and death, even against new variants.
- Vaccine Effectiveness Against Variants: Vaccine effectiveness against different variants varies, with some variants exhibiting greater ability to evade vaccine-induced immunity.
- Equitable Vaccine Access: Ensuring equitable access to vaccines globally is crucial to mitigate the impact of new variants. Disparities in vaccine access can lead to increased transmission and the emergence of new variants.
- Updated Vaccine Formulations: Developing and deploying updated vaccine formulations that target emerging variants is essential for maintaining high levels of protection.
Non-Pharmaceutical Interventions (NPIs): Layered Protections
Non-pharmaceutical interventions (NPIs) play a crucial role in slowing the spread of new variants and reducing case rates.
- Effectiveness of Different NPIs: The effectiveness of NPIs such as masking, social distancing, and improved hygiene practices varies depending on the context and the characteristics of the variant.
- Adapting NPI Strategies: Public health authorities must adapt NPI strategies based on the characteristics of circulating variants and community transmission levels.
- Public Health Communication: Clear and consistent public health communication is essential for encouraging adherence to NPIs and building public trust.
Testing and Contact Tracing: Containing Outbreaks
Widespread testing and effective contact tracing are crucial for identifying and containing outbreaks caused by new variants.
- Testing Methods: Various testing methods, including PCR and antigen tests, are available for detecting COVID-19 infection. Rapid testing is crucial for identifying cases quickly and initiating appropriate isolation measures.
- Importance of Timely Testing and Isolation: Prompt testing and isolation of positive cases are essential for preventing further transmission.
- Challenges in Contact Tracing: Effective contact tracing can be challenging, particularly in densely populated areas or settings with limited resources.
Conclusion
The impact of new COVID-19 variants on case rates is a complex issue influenced by several interrelated factors, including transmissibility, severity, immune evasion, and the effectiveness of public health interventions. Ongoing genomic surveillance, robust epidemiological modeling, and swift implementation of public health strategies, including vaccination, boosters, and NPIs, are vital for mitigating the impact of future COVID-19 variants. Staying informed about new variants and following public health recommendations, including vaccination, is crucial for protecting yourself and your community. Refer to resources like the WHO and CDC for the most up-to-date information on COVID-19 variants and public health guidance to help reduce COVID-19 case rates.
Featured Posts
-
 Ita Airways And Giro D Italia 2025 A Winning Partnership
May 31, 2025
Ita Airways And Giro D Italia 2025 A Winning Partnership
May 31, 2025 -
 Thursday Night Diamond Highlights District Champions And Playoff Qualifiers
May 31, 2025
Thursday Night Diamond Highlights District Champions And Playoff Qualifiers
May 31, 2025 -
 Haciosmanoglu Nun Macaristan Yolculugu Program Ve Goeruesmeler
May 31, 2025
Haciosmanoglu Nun Macaristan Yolculugu Program Ve Goeruesmeler
May 31, 2025 -
 Sanofi Expands Immunology Pipeline With Dren Bio Acquisition
May 31, 2025
Sanofi Expands Immunology Pipeline With Dren Bio Acquisition
May 31, 2025 -
 Decouvrir La Vie Et L Uvre D Arnarulunguaq Pionniere Inuit
May 31, 2025
Decouvrir La Vie Et L Uvre D Arnarulunguaq Pionniere Inuit
May 31, 2025
